Interventional Neuroradiology
Interventional neuroradiology specializes in minimally invasive procedures for the central nervous system. These procedures allow diagnostic and therapeutic measures to be carried out directly at the site of the disease without the need for open surgery. Our research focuses on the development and improvement of these minimally invasive procedures.
The aim is to improve patient care, increase the accuracy of diagnosis, and offer gentler treatment options. To this end, minimally invasive neuroradiological procedures' efficiency, safety, and effectiveness must be proven and optimized. This includes research into innovative imaging technologies, advances in catheter technology, and the evaluation of new materials and therapeutic approaches for neurovascular diseases, such as strokes, aneurysms, vascular malformations, or venous outflow disorders in the brain and spinal cord.
The research group for minimally invasive neuroradiological therapy works closely with the STIMULATE research campus and various industry partners.
Project
SOFINA (Simulation-based optimization of flow diverters for the treatment of intracranial aneurysms):
SOFINA (Simulationsgestützte Optimierung von Flussdivertoren für die Behandlung von intrakraniellen Aneurysmen):
The focus is on optimizing the treatment of intracranial aneurysms using flow diverters and researching ways to optimize the fluid dynamic treatment of intracranial aneurysms to shorten occlusion times, reduce the need for follow-up treatment, and further minimize the risk of ruptures. Furthermore, novel flow diverter designs and simulation-based planning and support software are being researched and developed.
Simulationen und Computational fluid dynamics (CFD):
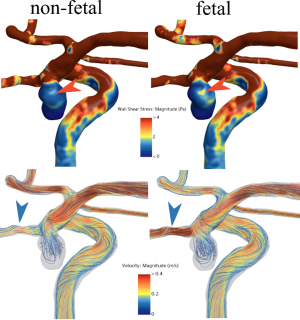
Together with the Medical Flows research group at the STIMULATE research campus, the aim is to use computer-aided simulations to predict blood flow in the brain vessels and thus assess the risk of vascular disease. Furthermore, various endovascular treatment scenarios are carried out virtually to investigate the influence of therapy on blood flow. Different implants and their positions can be compared, and the interaction between implants and blood flow can be characterized.
The various intracranial pathologies (e.g., aneurysms, arteriovenous malformations, and sinus stenoses) are converted into 3D models based on patient-specific medical image data. Subsequently, computational fluid dynamics methods investigate clinical questions regarding the blood flow behavior in the diseased vessels.
Fig.1 Qualitative hemodynamic comparison of fetal and non-fetal PcomA
Skull printing and 3D models:
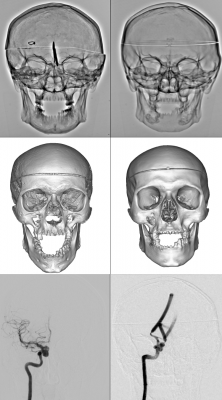
The use of 3D models in the context of interventional neuroradiology training, especially with a focus on cerebral vessels, offers many advantages for training and specialization.
The precise 3D representations of the brain vessels allow realistic simulations and specific interventions to be practiced. This enables prospective and experienced interventionalists to familiarize themselves with the complex vascular anatomy and improve their interventional skills.
The research focus is on producing realistic replicas of the human skull, particularly taking into account the radiographic representation and the original anatomical orientation of the 3D vascular models.
Fig. 2 X-ray images (top) and CT volume renderings (center) of the skull preparation (left) and the printed model (right), as well as a DSA comparison (bottom) of an actual aneurysm (left) to a corresponding printed vessel model in the printed skull (right).
Device testing and development:
Our research activities focus on testing and evaluating new materials for minimally invasive therapies for neurovascular diseases or other neurological conditions. In addition to model testing, we also carry out approval studies and post-marketing evaluations. To this end, we initiate or participate in our cross-center studies (see Clinical Trials). In addition, we develop new bioresorbable stents and flow diverters and the materials used for them as part of the EU-funded BIOMEND Doctoral Network.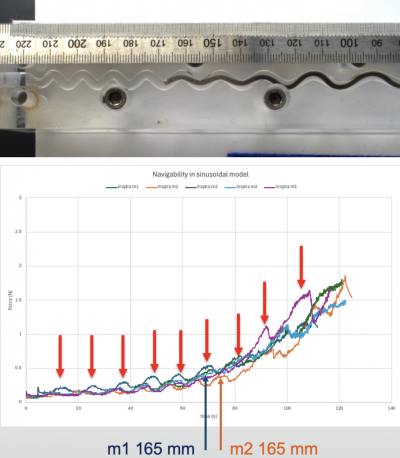
Fig. 3 Trackability test of an aspiration catheter (top) with the associated force development curve (bottom).
Employees
PhD students
Publications
|
Schwab, R., Kabbasch, C., Goertz, L. et al. The DERIVO 2 Heal Embolization Device in the Treatment of Ruptured and Unruptured Intracranial Aneurysms: a Retrospective Multicenter Study. Clin Neuroradiol (2024). https://doi.org/10.1007/s00062-024-01446-8 |
|
Böckmann, Julian, Klebingat, Stefan, Schwab, Roland, Behme, Daniel and Boese, Axel. "Evaluation of flushing parameters for clear view vascular endoscopy" Current Directions in Biomedical Engineering, vol. 9, no. 1, 2023, pp. 511-514. https://doi.org/10.1515/cdbme-2023-1128 |
|
Schwab R, Stahl J, Janiszewski R, et al |
|
Schwab R, Zschenderlein N, Boese A, et al |
|
Schwab R, Jan-Hendrik B, Behme D |
|
Schwab R, Stahl J, Stefan K, et al |
|
Schwab R, Stefan K, Diamandis E, et al |